#66 Rheumatology Emergencies w/ Dr Marce Ferrada
On this episode of Critical Care Time, we tackle the enigma - shrouded in mystery and caped in uncertainty - know as rheumatologic emergencies in the critically ill patient! We sit down with Dr. Marcela Ferrada - a QUADRUPLE boarded intensivist/rheumatologist/ID specialist and internist - who guides us through her approach to rheumatologic emergencies in the sickest of the sick. As we often do, we approach this via a pragmatic, cased-based journey for your listening pleasure. Please check it out, learn all you can, and as always - let us know your thoughts and leave a review!
“Rheumatism is the disease which imitates almost all others”
Dr. Marce Ferrada
University of Maryland
Intensivist, Rheumatologist & Infectious Disease Specialist
Why ICU Clinicians Need to Care About Rheumatology
Key message: Rheumatology is not just outpatient medicine.
The ICU is the final common pathway for severe rheumatologic disease.
ICU clinicians can save lives by recognizing inflammatory disease early.
Many cases are initially misdiagnosed as infection or sepsis.
High-Risk Triggers That Should Raise Suspicion
Young patients with severe illness and no clear infectious source
“Sepsis minus a bug”
Rapid AKI with active urine sediment
Cytopenias without explanation
Vasculitic features (rash, hemoptysis, neurologic events)
Unusual presentations:
MI in a 40-year-old
Stroke in a 20-year-old
Subglottic stenosis or unexplained airway disease
Key Terminology: Autoimmune vs Autoinflammatory
Rheumatologic disease is a broad category (includes OA, gout, RA, vasculitis).
Autoimmune diseases
Driven by adaptive immunity
Autoantibodies
Example: Systemic lupus erythematosus
Autoinflammatory diseases
Driven by innate immunity
Cytokine-mediated inflammation
Example: Familial Mediterranean fever
Organ-Based Clues about Rheumatologic Disease
Lung–kidney syndromes
Ocular inflammation
Oral or nasal ulcers
Skin rashes
Cartilage involvement
How Rheumatologic Disease Presents in the ICU
De novo presentation (first diagnosis in the ICU)
Mimics or co-occurs with infection
Catastrophic flare of known disease
Complications of chronic immunosuppression
Steroids and immunosuppression can be lifesaving—but dangerous if infection has not been reasonably excluded.
Send labs early—before steroids if possible, but don’t delay lifesaving therapy.
When to Suspect a Rheumatologic Emergency
ICU Red Flags
Persistent fever with negative cultures
Multiorgan dysfunction without microbial source
Unexplained cytopenias
Hemoptysis with new infiltrates
Rapid AKI + active urinary sediment
Known rheumatologic disease
Diagnostics: What to Send Early
Core labs
CBC with smear
CMP
Urinalysis with microscopy
Inflammatory markers (CRP, ESR, ferritin)
Autoimmune testing
ANA, dsDNA (SLE)
ANCA (PR3, MPO)
RF, anti-CCP
Complement levels (C3/C4)
Antiphospholipid antibodies
Cryoglobulins
Myositis antibody panels
Consultations
Consult Rheumatology early
Multidisciplinary care is essential:
Infectious Diseases
Nephrology
Hematology
Pulmonology
Steroids in Rheumatologic Emergencies
ICU clinicians use steroids daily—but rheumatologic emergencies require a different mindset.
General Principles
Life-threatening organ damage → treat immediately
Stable patient → await diagnostic clarity if feasible
Common Regimens
Moderate dose: Prednisone 1 mg/kg/day
Pulse therapy: Methylprednisolone 500–1000 mg IV daily × 3 days
Hydrocortisone reserved for adrenal insufficiency or shock
Case-Based ICU Discussion
Case 1: Scleroderma Renal Crisis
Diffuse systemic sclerosis → hypertensive emergency, AKI, TMA
Key management:ACE inhibitors ASAP
Avoid high-dose steroids
Anticipate difficult airway (microstomia, fibrosis)
Case 2: Catastrophic Antiphospholipid Syndrome (CAPS)
Catastrophic antiphospholipid syndrome
Rapid arterial + venous thrombosis
Multiorgan failure
Management
Therapeutic anticoagulation
High-dose steroids
Plasma exchange ± IVIG
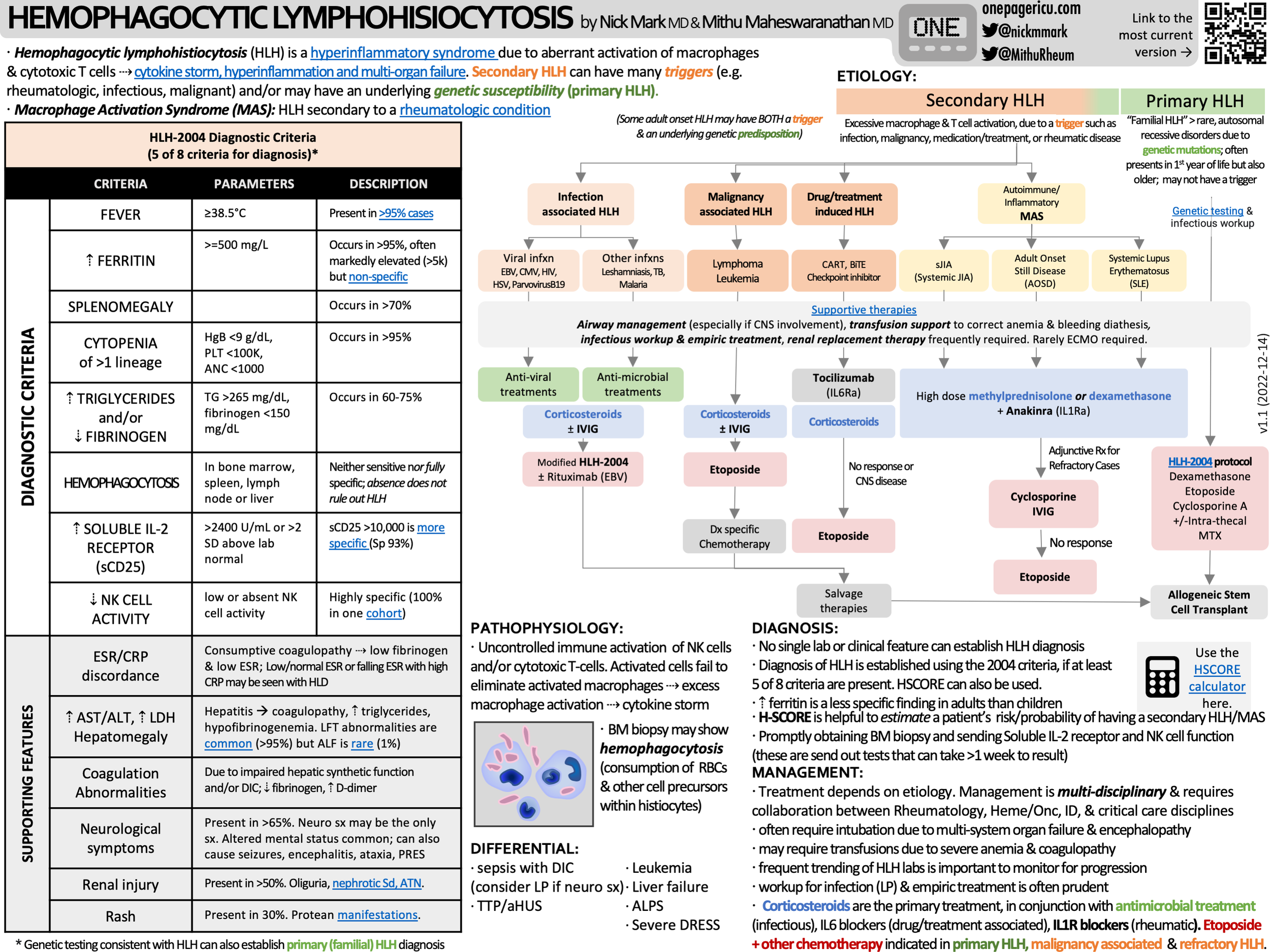
Case 3: MAS / Secondary HLH
Hemophagocytic lymphohistiocytosis
Fevers, pancytopenia, ferritin >50,000
Often triggered by rheumatologic disease
Management
High-dose steroids
IL-1 blockade (anakinra)
Consider etoposide in refractory cases
ICU OnePager Summary of HLH
Case 4: Diffuse Alveolar Hemorrhage (DAH)
Often no hemoptysis
Rapid hypoxia + anemia
Causes
ANCA-associated vasculitis
Lupus pneumonitis
Treatment
Pulse steroids
Rituximab or cyclophosphamide
Case 5: Pulmonary-Renal Syndrome
Goodpasture syndrome
DAH + rapidly progressive GN
Anti-GBM antibodies
Management
Steroids
Cyclophosphamide
Plasma exchange
Case 6: Severe Lupus Flare
Presentation
Neuropsychiatric lupus
Lupus nephritis
Pericardial tamponade
Management
Pulse steroids
Additional immunosuppressive therapy
Procedural intervention when needed
Case 7: VEXAS Syndrome
Presentation
Older men with fevers, cytopenias, thrombosis, organ-specific involvement (e.g., pneumonitis)
Often misdiagnosed as infection
Bone marrow vacuolization
UBA1 somatic mutation
Management
High-dose steroids
Other immunosuppressive therapies (e.g., IL-6 blockade)
Hematologic therapies (e.g., hypomethylating agents)
Pearl: VEXAS is recently described—but not rare. You’ve probably seen it.
Take-Home Messages
Rheumatologic emergencies appear more often than expected in the ICU.
Many cases are initially misdiagnosed as infection.
Develop a “spider sense” for inflammatory disease.
Send the right labs.
Consult Rheumatology early.
Early recognition saves lives.
Diseases to Know for the ICU
MAS / HLH
SLE
Pulmonary-renal syndromes
Diffuse alveolar hemorrhage
CAPS
VEXAS