#65 Bonus JC: RSI Trial
This Critical Care Time bonus is our ode to RSI... that is the RSI Trial! In this episode, we'll unpack all the important elements of the recently released RSI Trial by the Pragmatic Critical Care Research Group exploring whether there is a signal favoring etomidate vs ketamine for tracheal intubation of critically ill adults. Does one drug reign supreme? Is this practice changing, practice affirming or perhaps the devil's in the details? Listen, learn and let us know YOUR thoughts!
Trial design
This trial was done by the Pragmatic Critical Care Research Group, randomizing patients to either etomidate or ketamine for induction.
Inclusion: Patients were excluded if they were pregnant, prisoners, trauma patients, or had an immediate need for tracheal intubation that precluded randomization. Patients were also excluded if the treating clinicians determined that the use of ketamine or etomidate was either necessary or contraindicated.
Indication: Approximately 45-50% had hypoxemic respiratory failure, 15% had hypercarbic respiratory failure.
Location: Patients were intubated in the ED and ICU. The trial was conducted at 14 sites (6 EDs and 8 ICUs) in 6 medical centers across the United States.
Patients: They enrolled n=2365 critically ill adults. The patients were about 60% male. Median weight was 78 kg and median BMI was 27.
Indication: Approximately 45-50% had hypoxemic respiratory failure, 15% had hypercarbic respiratory failure.
Operator: About 60% were performed by by ED physicians and 40% by ICU physicians or anesthesiologist. Roughly 55% were done by residents, and 35% by fellows. Only 4-5% done by attendings.
Pre-oxygenation: About 45% were preoxygenated using a NRB. Only about 25% were preoxygeanted using NIPPV.
Paralytic: 31% of intubations were performed using Succinylcholine… yes they are still doing that. In 2025.
Intervention: Patients were randomized to ketamine or etomidate.
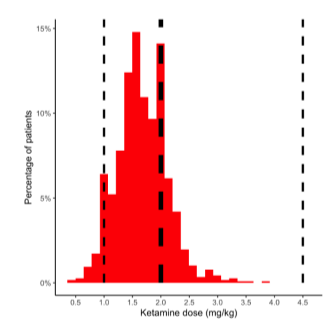
The median dose of ketamine was 140 mg or 1.6 mg/kg.
The median dose of etomidate was 20 mg or 0.28 mg/kg
Both were dosed using actual body weight, not ideal or predicted body weight.
More than half the patients received more that 1.5 mg/kg of ketamine (the usual dose). A significant fraction received much more as shown here:
From Supplemental Figure S2
Intubation: performed using VL was in 95% of cases. First pass success was achieved in 85% of cases.
Time: Compared to ketamine, etomidate was associated with significantly shorter time from induction to laryngoscopy (62 vs. 70 seconds) and to intubation (103 vs. 112 sec).
Hypothesis: they used such a monster dose of ketamine that it required two 10 cc syringes and thus took 8-9 seconds longer to push?!
Endpoints:
Primary Endpoint: The primary endpoint was in-hospital death by day 28, which occurred in 28.1% in the ketamine group and in 29.1% in the etomidate group. This was not significant.
Sidebar on power: They powered based on an expected 5.2% difference between the groups, which is a wildly high estimate! Doing a 10,000 patient trial powered to detect a 1% difference may have been impractical for cost/time reasons, but this 5% estimate likely doomed the trial to be negative.
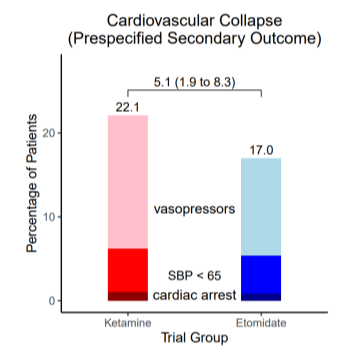
Secondary Endpoint: The secondary endpoint was a composite “cardiovascular collapse during intubation,” which was defined by the occurrence of any of the following events during the interval between induction of anesthesia and 2 minutes after tracheal intubation: a systolic blood pressure below 65 mm Hg, receipt of a new or increased dose of vasopressors, or cardiac arrest.
As with many composite endpoints, these are wildly dissimilar in terms of clinical importance! Cardiac arrest is much worse that requiring more vasopressors!
The composite of “Cardiovascular collapse” during intubation occurred in 22.1% in the ketamine group and in 17.0% in the etomidate group. That 5.1% difference was statistically significant!
This was entirely driven by the difference in “requiring increased dose of vasopressors” - precisely the endpoint with the least clinical importance:
From Supplemental Figure S8
Use of vasopressors prior to intubation was higher in the etomidate group:
Numerically more patients in the etomidate group were started on vasopressors prior to intubation (23% vs 20.9%) and more received prophylactic vasopressor with induction (19.7% vs 17.6%). This difference in practice may have led to fewer etomidate patients requiring a higher dose of vasopressors after induction, driving the difference in secondary endpoint!
So is the party over for ketamine?
Not for this guy, and probably not for the ICU either!
For the last decade, ketamine has been a wonder drug in the ICU. It’s the shiny new thing with a great reputation for safety. It was almost inevitable that more RCTs would deflate that bubble.
With these trials, there is a risk of drawing vast conclusions from half vast data.
This study was massively underpowered for clinically meaningful outcomes!
The composite endpoint was entirely driven by a difference in practice; providers expected hypotension with etomidate and pre-emptively started vasopressors!
Philippus Aureolus Theophrastus Bombastus von Hohenheim aka Paracelsus: the OG Toxicologist. He’s so fly even his hat has a hat.
This study is also a reminder of what paracelsus said 500 years ago “the dose makes the poison” (Latin: “dosis sola facit venenum“)!
Ketamine doses were unusually high!
The median dose was 1.6 mg/kg, meaning more than half the patients received more than the recommended dose (1.0 to 1.5 mg/kg)!
Furthermore, they used actual body weight (ABW) not predicted/ideal body weight (PBW/IBW)
There is controversy about whether actual or predicted body weight should be used when dosing ketamine. (In fairness to the authors, almost all prior studies used ABW)
The median BMI was 27 with an IQR of 23-32. That means that more than half the patients were overweight and a quarter were obese. These patients potentially got an even higher dose than necessary!
What does the pharmacology say?
Ketamine and etomidate are lipid-soluble, rapidly acting agents whose hemodynamic effects depend on central compartment volume
These principles may make IBW or PBW more physiologic than ABW in many patients.
A 150 kg person’s brain doesn’t weigh twice as much as a 75 kg person’s.
Lipophilic drugs like ketamine will eventually distribute to the whole body, but bolus pharmacokinetics are determined by central volume. Central compartment volume is likely similar in adults and in shock the central compartment volume shrinks, allowing a lower dose to be used.
Nick: “I typically use 1.5 mg/kg ABW up to 100 mg but don’t go higher. This means that I avoid overdosing larger patients, who likely don’t require a higher dose!”
In our recent airways controversy episode, our guest Jarrod Moser described the ketamine etomidate debate as the coke vs pepsi challenge. More one of personal preference than one being superior per se. Using that analogy, this study conclusively proves that forcing people to chug 2 liters of Coke is less good than sipping a normal amount of Pepsi.
-
RSI Trial (NEJM 2025)
-
-