#69 Mechanical Circulatory Support w/ Dr Bindu Akkanti
Folks this right here is a JAM PACKED episode of CCT goodness for you guys to enjoy! In this show for the ages we take a deep dive into the world of Mechanical Circulatory Support (MCS) and Cardiopulmonary Critical Care with one of the best in the biz, Dr. Bindu Akkanti! We will go through several fictional patients illustrating use cases, pitfalls and pearls of tools such as the balloon pump, ECMO and the microaxial flow devices used in ICUs all over the globe to help care for the sickest of the sick. If these tools ring a bell or if you are just interested in how we optimize care for these types of patients, give us a listen and let us know what you think!
Dr. Bindu Akkanti, MD
University of Texas Houston
Professor in the Department of Internal Medicine, Critical Care and the Graham Distinguished Professor in Pulmonary Medicine at McGovern Medical School at UTHealth Houston.
““Data! Data! Data! I can’t make bricks without clay.””
What is a “cardiopulmonary intensivist”?
A cardiopulmonary intensivist is a physician who specializes in the care of critically ill patients with severe heart and lung failure, especially when advanced support technologies are required.
Taxonomy of Mechanical Circulatory Support (MCS)
There are several different ways to categorize MCS:
Intra-corporeal vs extra-corporeal flow device (e.g. Impella vs ECMO)
Continuous vs Pulsatile (e.g. Impella vs IABP)
Centrifugal vs impeller pump (e.g. toilet bowl vs staircase)
RV vs LV support (LVAD vs RVAD, etc)
You can also think of MCS along a continuum from minimal to complete support.
Progression of increasing support: IABP —> Impella —> ECMO
This is analagous to oxygen delivery devices (nasal cannula —> HFNC —> NIPPV —> IMV); On a ventilator we often start at high level support (100% FiO2) then gradually de-escalate. We can do something similar with MCS by starting at high level support and then weaning.
The hemodynamic effects vary for of each MCS Devices:
Open source Hemodynamic Simulator by Nick Mark, MD. Source Code and documentation available here.
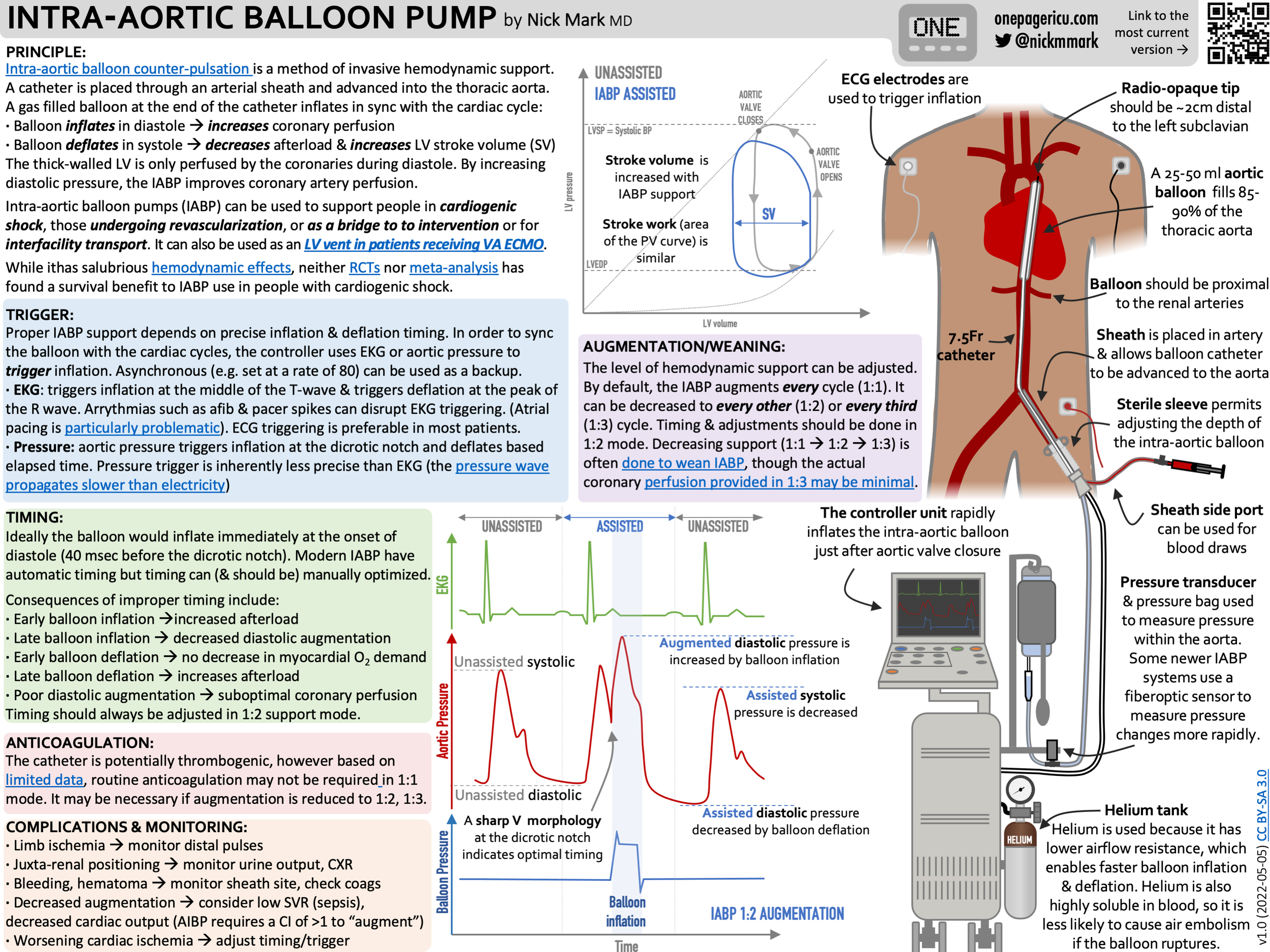
IABP OnePager by Nick Mark.
IABP
What it does
Inflates in diastole → augments coronary perfusion.
Deflates before systole → reduces afterload.
Where it still shines
LV-predominant shock
Mild–moderate severity
Preserved RV function
Need for temporizing support (e.g. in transporting to a higher level facility
IABP-SHOCK II reality
Despite the fact that IABP does not improve mortality in AMI shock, it:
is easy to place
fast
(relatively) inexpensive
has a low complication rate
buys time
Contraindications
Significant aortic regurgitation
Aortic dissection
Severe PAD / access limitations
How you know it’s working
Within hours:
lactate stabilizes or falls
pressor needs decrease
urine output improves
CI rises
Complications people miss
Limb ischemia
Migration
Poor timing
Understanding the IABP waveform is crucial:
Early inflation → ↑ afterload
Late inflation → lost augmentation
If hypertensive on IABP drop from 1:1 → 1:2 or 1:3.
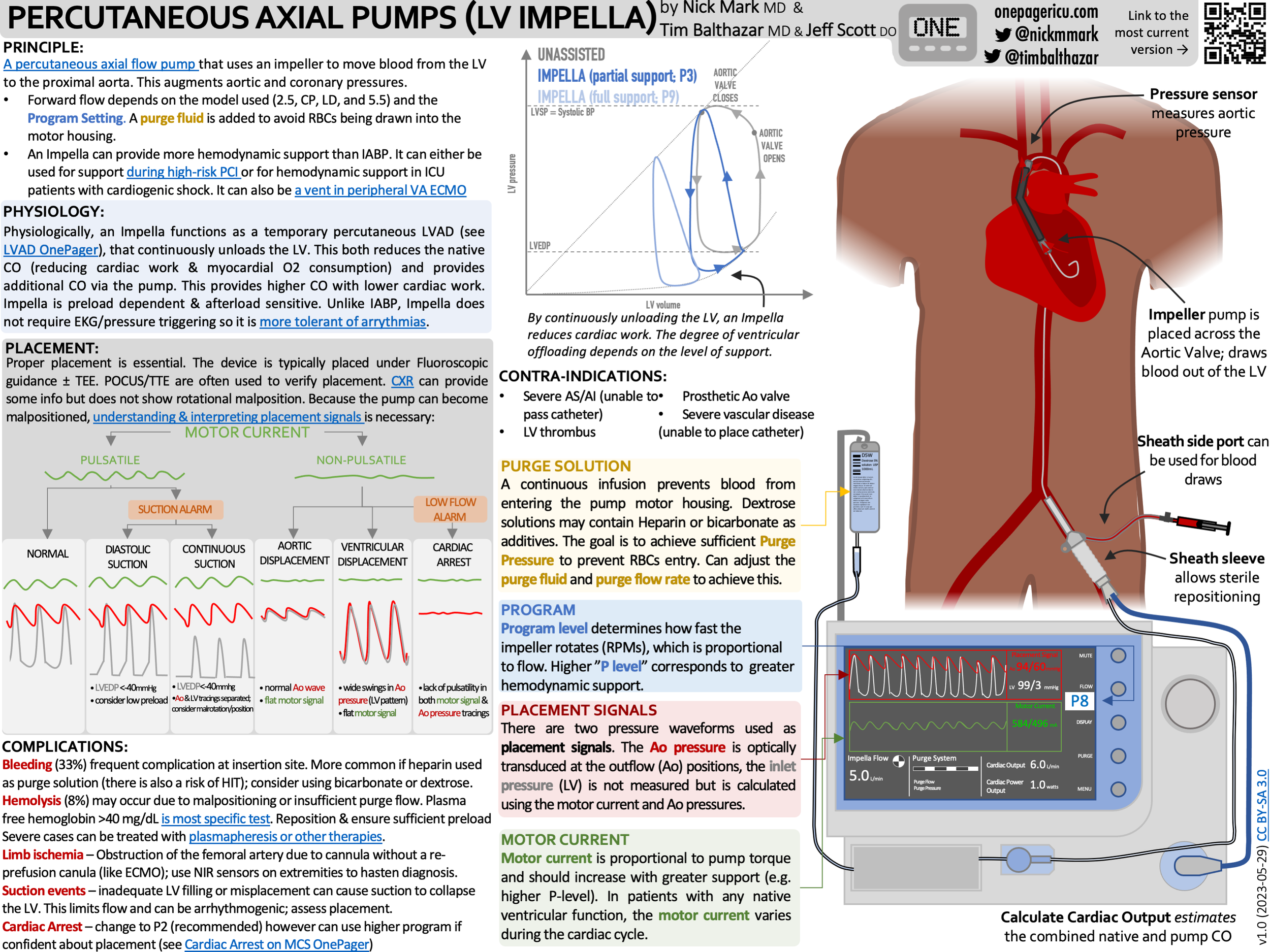
Impella
What hemodynamic phenotype is right:
high wedge
LV distension
pulmonary edema
PAPI preserved (use PAPI to evaluate RV function)
When an Impella is helpful
CVP/PCWP < 0.6 → RV probably tolerates LV unloading.
PAPI preserved
Significantly elevated wedge pressure
GET THE DATA you need. A PAC provides lots of useful data, including:
filling pressures
cardiac power
RV performance
If they need Impella → they likely need a PAC.
What gets better when it works
lactate ↓
MAP ↑
pulmonary pressures ↓
vent settings improve
Unique hazards of Impella
Hemolysis
Suction alarms
Malposition
Anticoagulation complexity
Alarms = information
Suction → low preload OR RV failure.
Device escalation
Impella CP → Impella 5.5 → ECMO.
Think continuum, like increasing FiO₂.
Mobility pearl: Axillary access = awake, rehab-friendly.
Pulmonary Artery Pulsatility Index (PAPI) Calculator
TandemHeart
What makes it different:
Drains left atrium → bypasses LV → strong forward flow (3.5–5 L/min).
Where it may outperform Impella
Need robust systemic output
LV too stiff or hostile
Septal defect scenarios
Risks
Big arterial sheaths → limb ischemia
Septal anatomy issues
Thrombus
Flow titration problem
Too much → LV distension
Too little → pulmonary edema persists
Veno-arterial ECMO
First hour checklist
Are cannulas correct?
Expected hemodynamic response?
Limb perfusion?
Hemolysis?
Use:
right radial arterial line
NIRS
frequent pulse checks
The LV distension problem: ECMO ↑ afterload.
Options:
medical unloading
Impella
surgical vent
atrial venting strategies
Harlequin syndrome
Native heart ejects poorly oxygenated blood to coronaries/brain → monitor right arm.
Recovery vs failure
Serial echo, pulsatility, end-organ trajectory.
Advanced configuration: Left atrial venoarterial ECMO
Drains RA and LA → decompresses both sides → may avoid extra devices.
Remember to get ALL the data:
Myocarditis isn’t always viral. Biopsy is recommended
ECPELLA
VA ECMO + Impella because LV is blowing up. This addreses one of the biggest hemodynamic limitations of ECMO: increased LV afterload.
Signs ECMO isn’t enough
worsening pulmonary edema
damp arterial waveform
minimal aortic valve opening
LV enlarging on echo
What ECPELLA adds
active LV venting
improved coronary perfusion
oxygenation + forward flow
Tradeoffs
More, bleeding, hemolysis, and potential for vascular complications
Requires tight coordination between ECMO and pump flows.
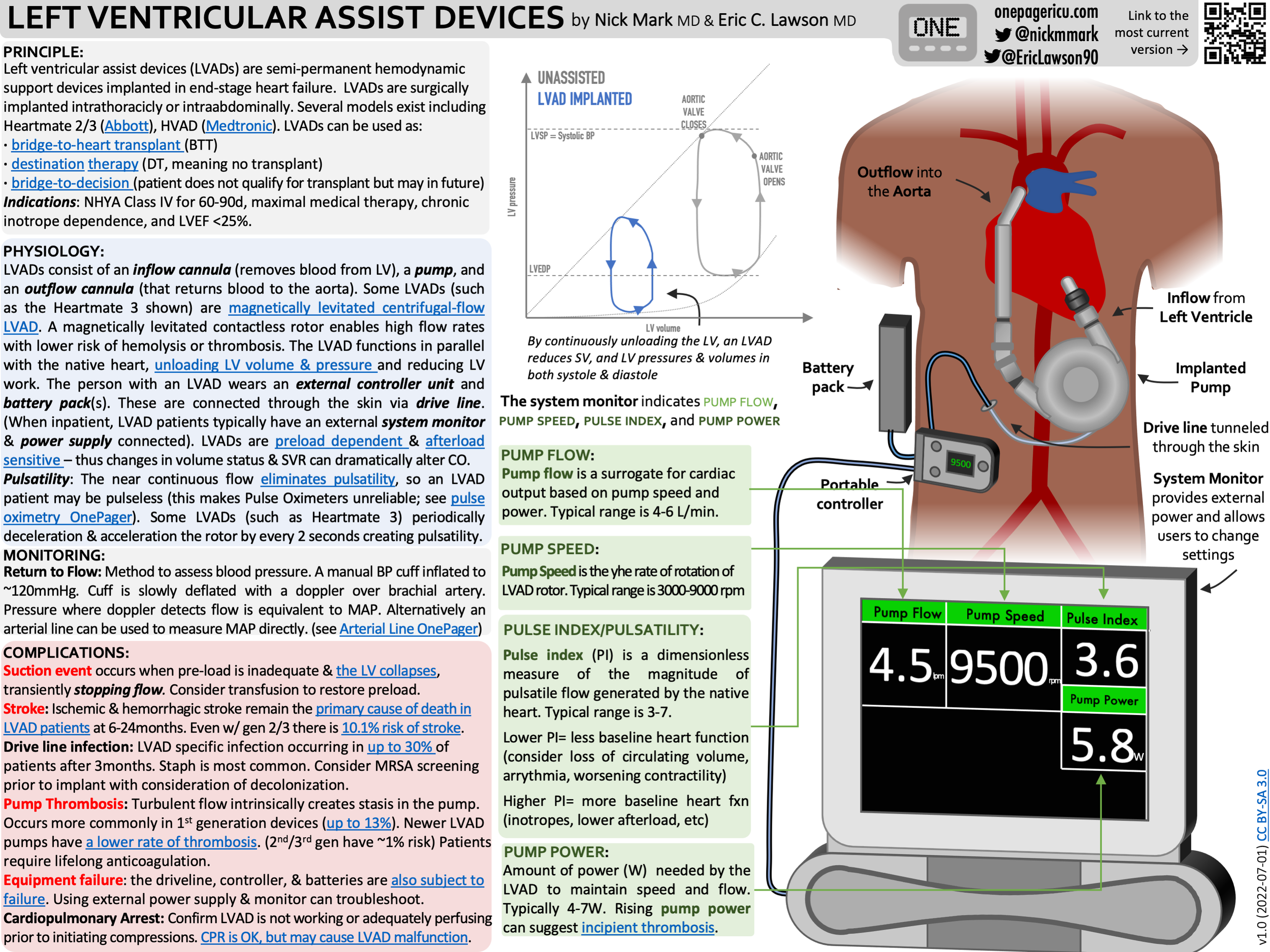
ICU OnePager guide to LVADs
LVAD Troubleshooting
Be wary of the big four complications
Suction event
Pump thrombosis
RV failure
Hypovolemia
Carefully monitor
mental status
lactate
cap refill
urine output
Red flags thrombosis
hemolysis labs
power changes
persistent low flow
Speed changes?
Small tweaks maybe.
Big decisions → call VAD team.
Monitoring: Echo + sometimes PAC.
General Advice for MCS:
1. Remember MCS is a spectrum
Just like ventilation → start big then de-escalate.
2. Get the Data and know the RV
The PAC is back, use it!
POCUS is also essential for placement, function, and to detect complications
Many device failures are actually RV failures.
3. Waveforms matter
Pulsatility provides important information.
Consider the waveform whenever troubleshooting IABP, Impella, etc
4. Early initiation improves odds of survival
5. Build systems
Shock teams, predefined triggers, mechanisms for rapid escalation.
CG shock team activation
Decide what would be offered/available
Quickly decide next steps/trigger
How to learn more:
Attend the Houston Shock conference (houstonshock.org) it’s free!