#61: Ventilator Basics
This week on Critical Care Time, Nick & Cyrus discuss the recent article in the Journal of Critical Care titled “Impact of initial jugular vein insertion site selection for central venous catheter placement on hemodialysis catheter complications.” Is this bunk or is this practice changing? Did they select the right population for this study or is the question they asked and answered... maybe not such a great question? We'll cover all this and more during this week's episode! Please take a listen, react, reach out & as always - don't forget to leave a review!
“Breath! You invisible poem! Back and forth, back and forth, exchanging in and out world space and Being.”
Why do we ventilate?
Primary Goals
Oxygenation: Maintain adequate PaO₂/SpO₂ to ensure oxygen delivery (DO₂).
Ventilation: Remove CO₂ and regulate pH.
Airway Protection: Plastic in the trachea when the airway can’t defend itself.
Other Key Goals
Avoid ventilator-induced lung injury (VILI) — keep pressures/volumes safe
Optimize comfort & synchrony — reduce work of breathing & dyssynchrony
Facilitate recovery — preserve muscle, avoid unnecessary sedation, plan for weaning
“Every strength is a weakness and every weakness is a strength”
The Language of the Ventilator
Ventilation vs Oxygenation
Ventilation = CO₂ removal → RR × tidal volume = minute ventilation
Oxygenation = FiO₂ + mean airway pressure
↑ pressure for ↑ time → ↑ oxygenation
(Mean Paw formula discussed)
| Concept | Question | Practical Meaning |
|---|---|---|
| Trigger | What starts the breath? | Time vs patient effort (flow/pressure trigger) |
| Cycle | What ends the breath? | Time, flow, or volume |
| Limit | What restricts the breath? | Pressure or volume limit |
| Assist vs Control | Who initiates the breath? | Patient-triggered assist vs machine control |
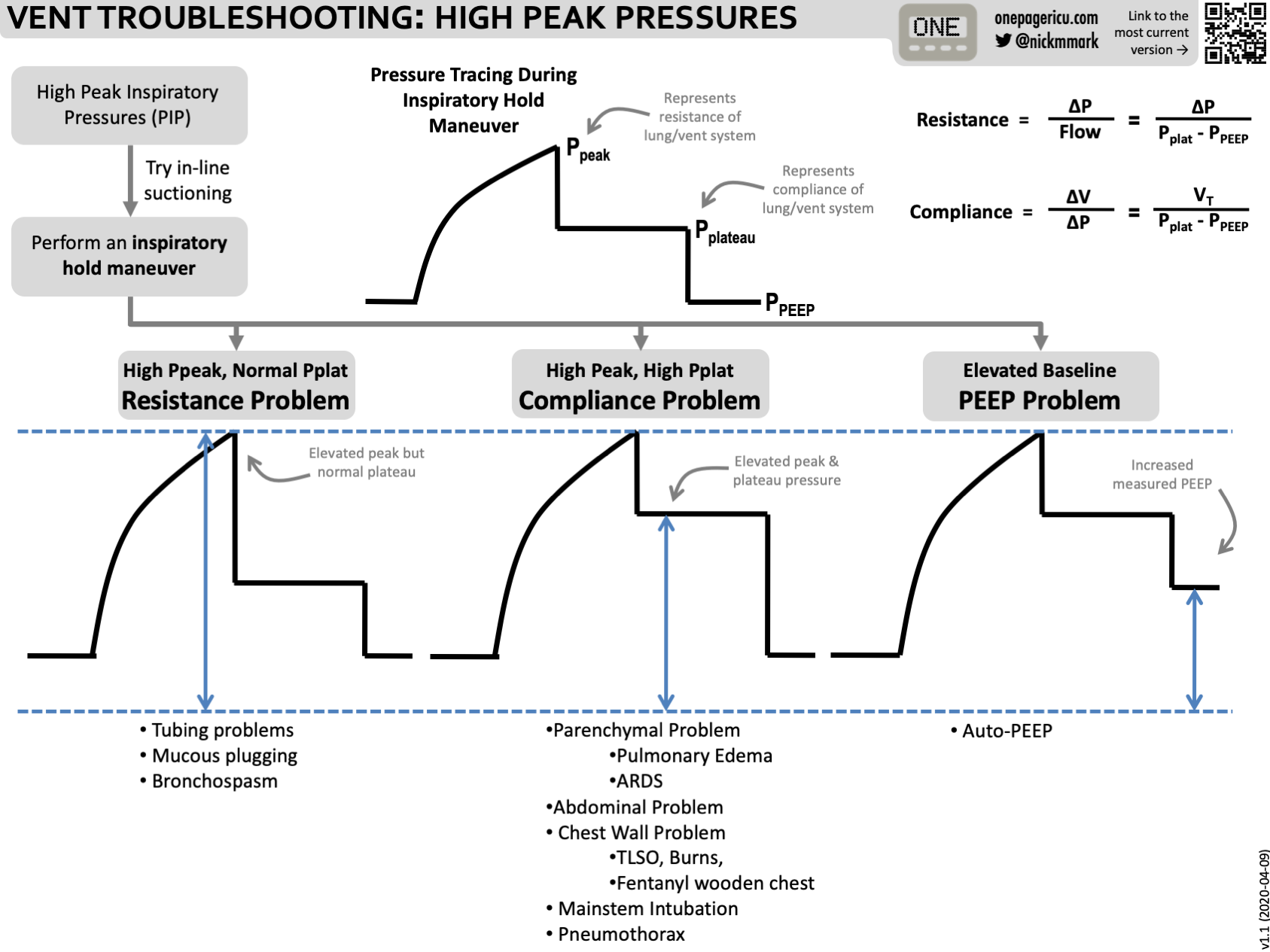
Pressures to Know
Peak Pressure — flow dependent → think resistance
Plateau Pressure — no flow → think compliance
Clinical rule: High pressure alarm? Decide peak vs plateau first
ICU OnePager guide to troubleshooting high ventilator pressures.
Core Settings
FiO₂, PEEP → oxygenation
RR, TV → ventilation / pH
Inspiratory pressure / time as applicable
Clinical heuristic: Think of vent settings like a phone number — group oxygenation variables (FiO₂/PEEP) and ventilation variables (RR/TV) with the blood gas.
Pearl:
If pH is the problem — fix ventilation.
If oxygenation is the problem — fix FiO₂/PEEP.
Common Ventilator Modes
Key point: There is no one mode to rule them all.
Volume Assist-Control (VC/AC)
Guarantees tidal volume
Watch for high pressures
Bread-and-butter for lung-protective ventilation (esp. ARDS)
Pressure Control (PC/AC)
Set pressure, time cycled
Good for low compliance lungs
Risk: variable volumes → hypoventilation
PRVC / VC+ (Hybrid)
Pressure-targeted with guaranteed tidal volume
Good comfort & lower peak pressures
Caution: In strong spontaneous breathing, ventilator may reduce support → ↑ WOB
Useful general mode; not ideal in ARDS
Pressure Support
Patient-triggered, no set rate
Used for spontaneous breathing trials & weaning
Brief Mentions
SIMV
Historically weaning — now generally inferior to PS/SBT
Still used in postop/surgical ICU patients without lung disease
Nick: I love this mode in people having hiccups
APRV
CPAP with brief release
Potential benefit in select spontaneously breathing ARDS patients
Steep learning curve, limited evidence, challenging for handoffs
Future “controversy” episode potential!
Big takeaway: Every mode has trade-offs — goal is matching mode to physiology & patient state.
Safety & Pitfalls
Avoid VILI
Barotrauma, volutrauma, atelectrauma, biotrauma
Oxygen toxicity
Common Errors
Treating numbers instead of physiology
Overusing FiO₂ instead of optimizing PEEP
Sedating dyssynchrony instead of understanding it
Forgetting permissive hypercapnia is often intentional
“Perfection is the enemy of good”
-
-
ARDS
-
ICU OnePager Summary of Ventilator Modes