#55 Cirrhosis and Variceal GI Bleeds
On this week's episode of Critical Care Time, Dr. David Dulaney rounds out GI bleeds in the ICU by taking on cirrhosis & variceal bleeds! During this show we discuss the unique challenge associated with managing a patient with cirrhosis - specifically focusing on the coagulopathy of advanced liver disease. We then delve into the nuances associated with managing a variceal bleed, both in terms of the unique critical care elements but also the challenges faced by the endoscopist when trying to saves these patients in extremis. Tune in, leave us a review and most importantly - leave us some feedback!
Despite progress, variceal bleeds remain deadly
Acute variceal hemorrhage (AVH) remains among the most lethal GI bleeds.
Contemporary series/guidelines cite ~10–20% 6-week mortality, higher in Child-Pugh C or where multidisciplinary care is limited.
Early vasoactive drug + antibiotics + early endoscopy have lowered mortality, but risk remains substantial.
The single biggest “mortality mover” the past decade: packaging early vasoactive therapy, antibiotic prophylaxis, restrictive transfusion, and timely endoscopy (≤12 h)—and for the right patient, early-TIPS.
Understanding cirrhosis pathophysiology
Portal hypertension drives varices; clinically significant portal HTN (CSPH) at HVPG ≥10 mmHg is the threshold for decompensation events (variceal bleed, ascites, HE).
Compensated vs decompensated: decompensation = overt portal HTN complications (variceal hemorrhage, ascites, HE). Prognosis shifts dramatically once decompensation occurs.
Other ICU syndromes to anticipate in cirrhosis:
Spontaneous Bacterial Peritonitis (SBP)
Severe Hepatic Encephalopathy (HE)
HRS-AKI
Sepsis with low-SVR shock
Hemodynamics & pressors: cirrhotics are hyperdynamic/low-SVR; treat shock with norepinephrine first-line per sepsis guidance; consider adjunct vasopressin if refractory (also lowers portal flow/pressure, but watch ischemic risks and do not use as a substitute for splanchnic vasoactives).
“Auto-anticoagulated” myth: cirrhosis = rebalanced hemostasis (losses in pro- and anti-coagulants). Lab INR poorly reflects bleeding risk; VET (TEG/ROTEM) often more informative and can reduce product use for procedures without increasing bleeding.
Initial assessment & stabilization
Airway
Who to intubate?
Intubate for active hematemesis, impaired consciousness (HE), or when planning endoscopy with high aspiration risk. Observational data/linkage analyses suggest prophylactic intubation can increase pneumonia and possibly mortality; if you intubate, do it deliberately and early (not a crash tube mid-scope), and extubate early once safe.
Induction pearls in HE: Avoid overly deep sedation; consider etomidate or ketamine titrated; minimize hypotension; be ready for massive airway contamination—suction aggressively; large-bore OG after ETT for decompression. (Expert consensus/guideline-concordant.) Connected Culture Expo
Access & monitoring
Large-bore peripheral IVs are fine to start; place arterial line early; central access as needed. Do not “correct the INR” solely to place lines; if worried, use VET-guided strategy.
Transfusion strategy (RBCs & components)
Restrictive RBC transfusion: target Hgb ~7 g/dL (higher threshold if MI/ongoing ischemia). Restriction improves outcomes vs liberal strategy in UGIB and avoids raising portal pressures that can worsen bleeding.
Avoid FFP to “fix” INR; it does not correct hemostasis and can worsen portal pressures. Consider cryoprecipitate if fibrinogen <100–120 mg/dL and platelets if <50k for procedures/ongoing bleeding—prefer VET guidance when available.
Antifibrinolytic? TXA
HALT-IT (24,000+ pts UGIB) was negative for mortality and showed ↑ seizures/VTE; routine TXA not recommended. PMC
BUT: a 2024 Hepatology RCT in cirrhotics with UGIB (CTP B/C; >85% variceal sources) found lower failure to control bleeding by day 5 and better sustained hemostasis with TXA (esp. first-time EVL). Consider case-by-case in decompensated cirrhotics with EV bleeding after weighing risks.
Vasoactive drugs (start now, don’t wait)
Octreotide: 50 µg IV bolus, then 50 µg/h infusion (or 25–50 µg/h).
Terlipressin (where available): 2 mg IV q4h for 48 h, then 1 mg q4h up to 2–5 days. (Doses per AASLD Table.)
Multiple trials/meta-analyses: octreotide ≈ terlipressin for bleeding control; choose based on availability/contraindications. (Note: US approval of terlipressin is for HRS-AKI, not specifically AVH.)
Antibiotics (give early)
Rationale: Bleeding + cirrhosis → bacterial translocation & immunodysfunction → infections drive rebleeding & mortality.
Recommended: ceftriaxone 1 g IV q24h for up to 5–7 days (can stop earlier once hemostasis achieved and vasoactives off). RCTs show ceftriaxone > norfloxacin in advanced cirrhosis; several meta-analyses support prophylaxis. (Resistance patterns and MDRO concerns are evolving; de-escalate when safe.)
PPI & prokinetic
Empiric PPI reasonable before endoscopy (diagnosis undifferentiated); stop if confirm portal hypertensive bleeding (some give a short PPI course after EVL for post-band ulcers/pain).
Erythromycin 250 mg IV 20–90 min pre-EGD improves visualization, reduces repeat EGD and LOS—use if significant hematemesis/clot burden.
Timing & conduct of endoscopy
Goal: Endoscopy within 12 hours of presentation after initial resuscitation/airway stabilization and after vasoactive + antibiotics have started.
Primary endoscopic therapy: EVL (banding) for esophageal varices. If visualization is poor, lavage + erythromycin; if active torrential bleeding, consider hemostatic powder as a bridge (rescue/adjunct; off-label).
When banding fails
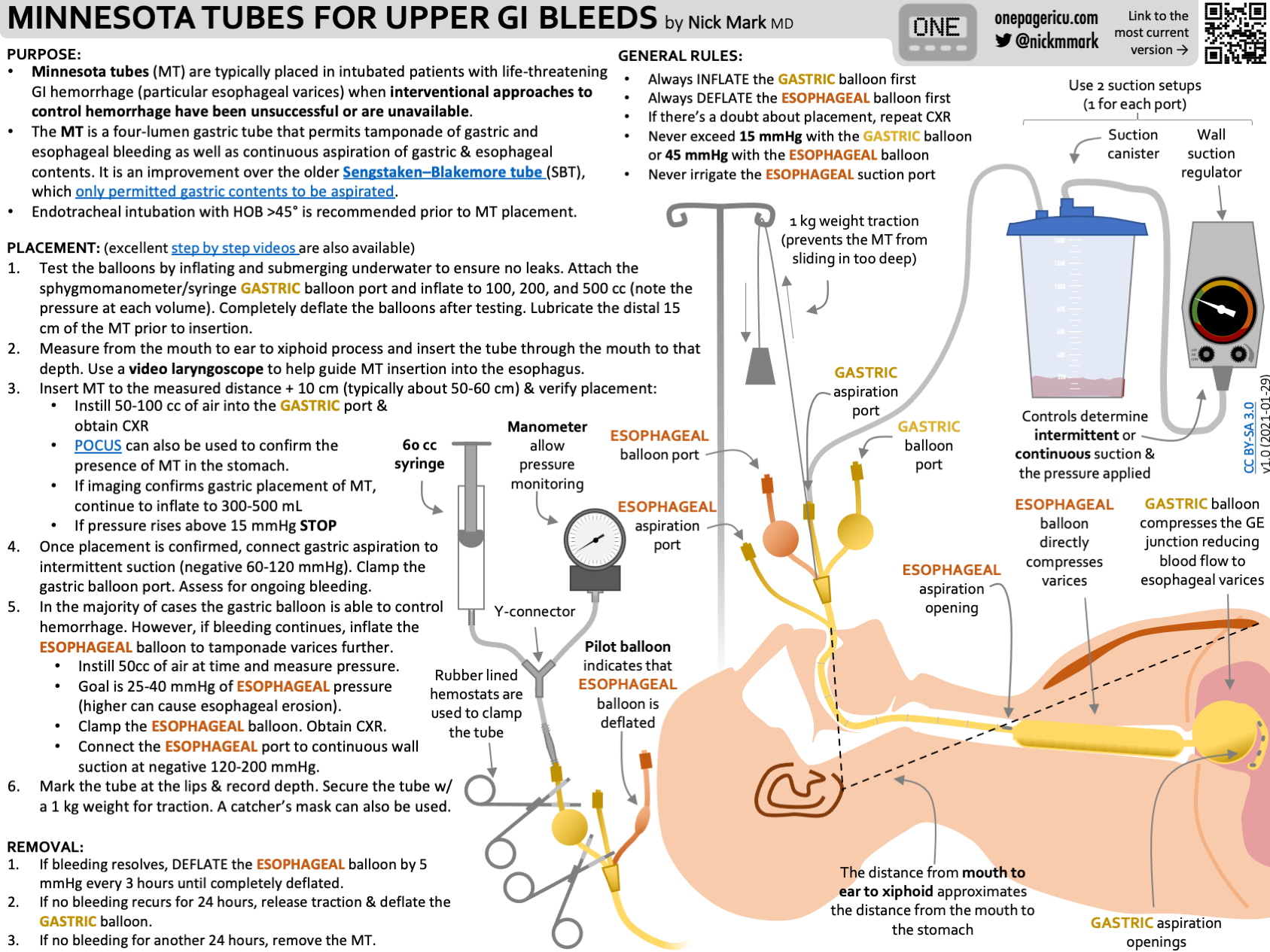
Balloon tamponade (Sengstaken-Blakemore/Minnesota)
Effective as temporary bridge (control in ~50–90% depending on experience), but complication-prone (aspiration, necrosis) → intubate first; confirm gastric balloon is in stomach before full inflation; apply traction.
Fully-covered self-expanding esophageal stent (FC-SEMS)
Alternative to tamponade: RCT & meta-analyses suggest better bleeding control and fewer adverse events vs balloon tamponade in refractory EV bleeding; still a bridge to TIPS or definitive therapy. Requires endoscopic expertise/availability.
ICU OnePager approach to Minnesota Tube Placement
“Early-TIPS” (pre-emptive) vs rescue/salvage TIPS
Who benefits from early-TIPS? High-risk patients: Child-Pugh C 10–13 or Child-Pugh B with active bleeding at endoscopy. Place within 72 h (ideally <24 h). RCTs show improved control/rebleeding and survival advantage. Target PSG <12 mmHg or ≥50–60% reduction.
Rescue TIPS: when rebleeding during index admission after initial hemostasis.
Salvage TIPS: for persistent/uncontrollable bleeding despite optimal endoscopic/medical therapy.
Gastric varices (a different beast)
Sarin classification: GOV1 (lesser curvature extension) behaves like EV; GOV2 (fundus), IGV1 (fundus alone), IGV2 (distal stomach) behave differently. Always visualize the fundus.
Therapy:
Fundal varices: cyanoacrylate/glue ± coils/EUS-guided therapy when expertise exists; otherwise TIPS (± BRTO depending on anatomy/shunt).
For rebleeding or lack of expertise, proceed to TIPS ± variceal obliteration.
Post-bleed “steady state”
Vasoactive duration: continue octreotide/terlipressin for 2–5 days after hemostasis for portal hypertensive bleeding. Outpatients without acute bleed do not get octreotide.
Non-selective beta-blockers (NSBB): start/restart after vasoactive infusion stops; carvedilol is often favored (greater HVPG reduction) where tolerated; EVL for those with contraindication/intolerance. Secondary prophylaxis is NSBB + EVL.
Surveillance endoscopy: q2–4 weeks until eradication, then 6 months, then q12 months.
Transplant referral: consider early in decompensated patients; “test answer” MELD ~15 triggers referral thinking, but practical listing thresholds vary by region/exception points.
Pearls from the episode
Don’t chase the INR. Use TEG/ROTEM if available.
Restrict the blood. Over-transfusion raises portal pressure; stick near 7 g/dL.
Antibiotics matter. Start ceftriaxone early; reassess daily; de-escalate when appropriate.
Think early-TIPS in the right patient (Child-B active bleed or Child-C 10–13). Call IR early.
When endoscopic control is failing, FC-SEMS is may be safer & more effective than balloon tamponade as a bridge.
-
-
Vasopressors
-
GeoSentinel Surveillance Network
IDSA Guidelines on Fever in the ICU