#59 Airway Controversies w/ Dr Jarrod Mosier, MD
Join us this week on Critical Care Time as we take on Airway Controversies with Dr. Jarrod Mosier - course director for The Difficult Airway Course: Critical Care! We talk induction agents, pre-oxygenation and cover so much more in this episode!
If you love this - consider attending the upcoming Difficult Airway Course at the Manchester Grand Hyatt in sunny San Diego, California from November 14th to the 16th and use our Discount Code CCTIME25 at checkout and save $250!
Guest: Jarrod Mosier, MD
Professor of Emergency Medicine & Medicine, University of Arizona; Intensivist, ECMO Director, Course Director of The Difficult Airway Course: Critical Care
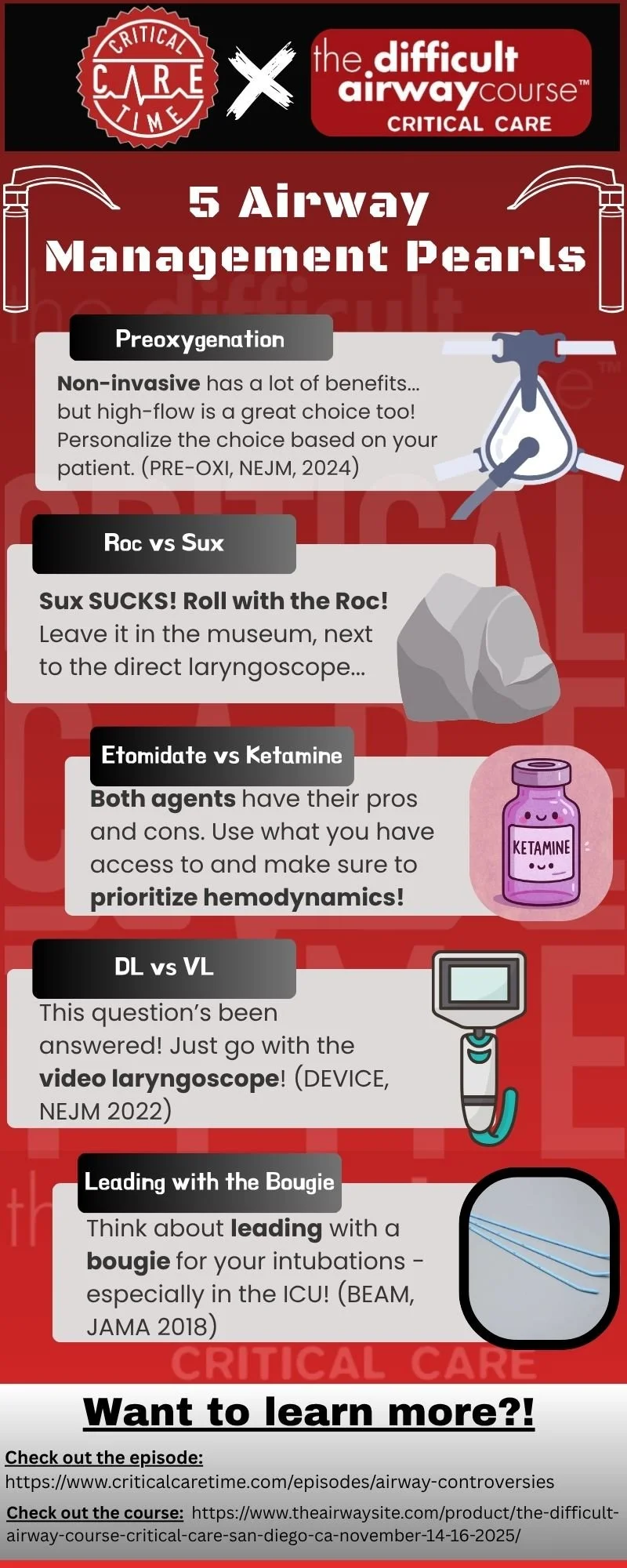
Airway Controversies
In this episode of Critical Care Time, we dive deep into airway controversies—the places where smart, experienced clinicians disagree about best practice. We’re joined by Dr. Jarrod Mosier, who quite literally wrote the book on airway management. Together, we cover the hottest debates in preoxygenation, induction, paralytics, devices, and more.
Recurring theme: the enemy of good is better—sometimes striving for the “perfect” strategy can be less important than getting it right, safely, and consistently.
1. Preoxygenation & Apneic Oxygenation
Key Question: NRB vs BVM vs HFNC vs NIPPV — is there a “best” preoxygenation tool?
Good pre-oxygenation consists of three parts:
Adequate FRC
Good denitrogenation
Minimal shunt
The evidence is mixed:
PRE-OXI (NEJM 2024): NIPPV > BVM for preoxygenation.
PREVENT (NEJM 2019): BVM > no-ventilation.
FELLOW (AJRCCM 2016): Apneic O₂ no benefit.
FLORALI-II (Lancet 2019): neither NIPPV or HFNC reduced risk of hypoxemia
Silva et al. 2017 meta-analysis: mixed findings
Verdict: Personalize. NIPPV is increasingly favored, but HFNC/apneic oxygenation may still play a role.
📄 Mosier 2024 review | UpToDate: Physiologically Difficult Airway
2. Paralytic Choice: Rocuronium vs Succinylcholine
Controversy: Is succinylcholine still relevant in 2025?
Evidence:
Rocuronium - when properly dosed (1.2 mg/kg NOT 0.6 mg/kg) - has comperably fast onset to succinylcholine.
Because it is non-depolarizing, rocuronium may theoretically cause less O2 consumption, leading to less hypoxemia.
Rocuronium is reversible with sugammadex; safer profile.
Verdict: Rocuronium preferred. “Sux belongs in a museum, right next to the direct laryngoscope.”
3. Induction Agent: Ketamine vs Etomidate
Evidence:
RCTs:
Prehospital/ED RCT Critical Care 2009 (multicenter; n=~470): Etomidate 0.3 mg/kg vs ketamine 2 mg/kg. No difference in 28-day mortality or organ failure; etomidate caused more adrenal insufficiency (86% vs 48%); intubating conditions were similar.
Observational studies:
Large Observational US database study by Wunsch et al, found Etomidate associated with higher hospital mortality vs ketamine after adjustment. (Caveat: Observational; association, not causation.)
MATCH-IT trial - anesthesia intubations in Texas hospital. Higher 7 day mortality but similar 28 day mortality.
Sepsis-specific meta-analyses (conflicting):
2012 meta-analysis (CCM): etomidate linked to higher mortality and adrenal insufficiency in sepsis; on the other hand a 2015 meta-analysis (CHEST) found no mortality increase with single-dose etomidate.
Meta-analyses:
Systematic review/meta-analysis (2022, 9 studies; ED/prehospital): Etomidate ↓ post-induction hypotension (OR 0.53) with no difference in first-pass success.
Bayesian meta-analysis (2024, 7 RCTs + 1 matched; ICU/ED/prehospital, n=2,978):
83% probability ketamine reduces mortality vs etomidate (RR 0.93; 95% CrI 0.79–1.08); no differences in SOFA, VFDs, vasopressor-free days, or first-pass success.
Etomidate ↓ immediate hypotension but ↑ adrenal suppression (though this was only when much higher doses were used as continuous infusions; likely not applicable to modern induction doses.
Observational studies/meta-analyses: ketamine possibly lower mortality, though significant methodological limitations.
Verdict:
Nick: favors ketamine (“pay now vs pay later” with hypotension)
Jarrod: both drugs fine; focus should be fixing hemodynamics before intubation.
This is a Coke vs Pepsi situation: everyone has a preference but they are both sugar water. In blinded taste tests people can’t actually tell them apart.
4. Video Laryngoscopy (VL) vs Direct Laryngoscopy (DL)
Evidence:
DEVICE RCT (2022):
n=1417 ED and ICU patients
Stopped early for efficacy: higher first-pass success with VL (85.1% vs 70.8%); severe complications similar between groups (21.4% vs 20.9%).
Synthesis of studies: 2024 Critical Care updated meta-analysis of RCTs (ICU/ED; 14 trials; n=3,981)
VL improved first-pass success (RR 1.12, 95% CI 1.04–1.20) and reduced esophageal intubation (RR 0.44) and aspiration (RR 0.63). Authors conclude VL is the more effective and safer strategy in critically ill patients overall.
Verdict:
VL should be first-line in critically ill patients.
Not only are you more likely to succeed with intubation using VL, but it allows a shared mental model (we can all see the anatomy), and improved QI/QA (we can review recordings).
5. First-Line Bougie
Evidence:
BEAM trial (JAMA 2018): Bougie ↑ success (96% vs 82%).
Verdict: Strong case for routine first-attempt bougie use, especially in ED/ICU.
Key Takeaways
Airway management is full of gray zones.
Personalization—patient physiology, operator experience, setting—matters more than dogma.
As Dr. Mosier put it: “Don’t expect your induction drug to bail out your hemodynamics—fix those before you intubate.”
Sponsor:
If you want to learn more about managing difficult airways we highly recommend you check out our sponsor: The Difficult Airway Course: Critical Care
The Difficult Airway Course: Critical Care™ focuses exclusively on the airway challenges posed by critically ill inpatients. This advanced course is designed for intensivists and for hospitalists who are responsible for emergency airway management of acute inpatients.
Build mastery and confidence in:
How to predict a difficult airway and prevent a failed airway
When - and when NOT - to use medications
How to perform an awake intubation
Tube exchange and extubation of the difficult airway
Practical strategies in crisis management and human factors
Featuring a dynamic and interactive learning environment, the Course emphasizes airway assessment and decision-making to build the capacity to manage all airway situations — and to do so with great confidence.
Critical Care Time listeners get a $250 discount when they register, using code CCTIME25 at checkout
-
ANDROMEDA-SHOCK
-
-